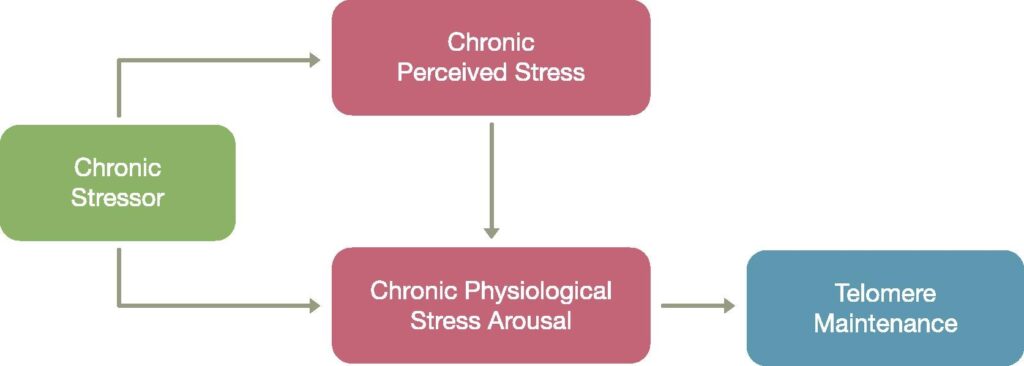
A meta-analysis of nearly 9,000 people confirms that the level of perceived stress is associated with somewhat shorter telomere length, although this correlation is very low (r ≈ -0,06 age-adjusted). However, recent evidence suggests that it is not so much psychological stress in isolationbut the integrated response to stress -how the body processes it at the cellular and systemic level - how it is processed by the organism which could have a major impact on longevity at the telomeric level.
Previous studies had already shown that the chronic and perceived stress is associated with shorter telomeres and reduced telomerase activity in immune cells. In highly stressed individuals, such as mothers caring for chronically ill children, telomeres may shorten by up to the equivalent of an additional decade of ageing.
A longitudinal follow-up analysis in the MESA cohort (10 years, 1,158 people) showed that those who moved from low to high levels of chronic stress experienced significantly greater telomeric shortening (-0.054 units).
In addition, a review of 15 studies focusing on middle-aged and older adults revealed that not all psychological and biological stress response factors are equally affected by stress.. Certain components - such as anticipation of danger, perception of control or physiological resilience - are particularly important determinants of the rate of telomeric shortening.
On the other hand, research on the integrated mitochondrial stress response (ISR^mt) has emerged as a highly relevant pathway. According to a recent review (2024/2025), this response activates an adaptive mechanism regulated by ATF4 that in early stages may protect against ageing-associated diseases, promoting cell survival and metabolic well-being.
In summary, although perceived stress has a small effect on telomeres, it is the most important factor in telomere length. integrated stress response -which includes psychological, metabolic, hormonal and cellular aspects - is likely to most accurately determine the rate of biological ageing and telomere length.
Managing stress is not just about avoiding feeling overwhelmed, it is about improve physiological resilienceHealthy responses in cortisol, inflammation, mitochondrial function and oxidative network.
Effective interventions are those that combine emotional management (psychoeducation, mindfulness, social support) with healthy habits (regular exercise, sleep, balanced diet).
Stimulating the adaptive response to mitochondrial stress could be a novel strategy in longevity, although human clinical trials are still pending.
The most effective treatments for reversing or modulating the integrated biological stress response -which includes activation of the HHA (hypothalamic-pituitary-adrenal) axis, systemic inflammation, oxidative stress, mitochondrial imbalance and immunometabolic dysfunction- go beyond the subjective relief of psychological stress. They focus on restoring deep physiological homeostasis. Here are the most scientifically supported approaches:
1. Neurobiological and regenerative modulation therapies
- Neuromodulation therapy REAC (Radio Electric Asymmetric Conveyer)
Redirects the adaptive response of the autonomic nervous system. Studies show reduced oxidative stress, improved vagal tone and sympathetic-parasympathetic balance. - Transcranial stimulation direct current switching (tDCS)
Regulates neuronal connectivity and may help reset hyperactivation patterns of the HHA axis. Promotes neuroplasticity and biological resilience. - Mitochondrial bioenergetic therapies
As the photobiomodulation (low level laser) o red light therapywhich stimulate mitochondrial function, reduce free radicals and modulate the inflammatory response. - Hyperbaric chamber (HBOT)
Improves tissue oxygenation, reduces chronic low-grade inflammation and promotes neurogenesis and angiogenesis. Helps reverse damage from systemic stress.
2. Adaptogens and nutraceuticals with mitochondrial and hormonal action
- Ashwagandha, Rhodiola and Eleutherococcus
They normalise cortisol levels and reduce HHA axis hypersensitivity, without sedation or dependence. - Magnesium, L-theanine and tryptophan
They act on the neurochemistry of the autonomic nervous system and serotonergic balance. - Omega-3, resveratrol, PQQ and Coenzyme Q10
They have direct effects on mitochondrial biogenesis and reduction of cellular oxidative stress.
3. Mind-body therapies with proven systemic effects
- Mindfulness with a focus on interoception
It not only reduces the perception of stress, but also improves markers of inflammation (IL-6, CRP), telomerase and parasympathetic activity. - Slow diaphragmatic breathing (cardiac coherence)
It activates the vagus nerve, improves heart rate variability (HRV) and regulates the HHA axis. - Somatic therapies (SRT, neurofeedback, HRV biofeedback)
They help to deprogram chronic stress response patterns at subcortical and autonomic levels.
4. Hormonal and epigenetic therapies (where clinically indicated)
- Bioidentical DHEA and melatonin replacement
In phases of HHA axis depletion (chronic stress), these treatments restore the anabolic-catabolic balance and modulate the immune system. - Epigenetic modulation (e.g. NR, NMN, spermidine)
They influence gene expression related to the cellular response to stress-induced damage.
5. Personalised protocols based on biomarkers
- The use of diurnal cortisol, pro-inflammatory cytokines (IL-6, TNF-α), mitochondrial metabolomics y HRV to design specific treatments.
The key is not to "calm" the stress, but rather to re-educating biology to regain adaptive flexibility. This involves interventions on the autonomic nervous system, mitochondrial metabolism, the immune system, chronic inflammation and neuroplasticity.






